Introduction
Definition of absenteeism
Absenteeism refers to periods when employees are absent from their workstations. In the hospital environment, this poses specific challenges. Absenteeism can be caused by illness, personal problems or difficult working conditions.
Current context and importance of the subject
The rate of absenteeism in hospitals is alarming. In 2020, the rate in French hospitals averaged between 9.5% and 11.5%, according to figures from the French Hospital Federation survey. According to another recent survey (2022), this rate has a significant impact on the operation of healthcare facilities. Continuity of care and efficiency of services are very often compromised. The number of vacancies for state-qualified nurses has risen from 7.5% to 13.1% in three years in medico-social establishments and services (ESMS), and from 3% to 6.6% in healthcare establishments, excluding university hospitals.
In 2016, the iFRAP Foundation also published a ranking of absenteeism in French hospitals and teaching hospitals for 2013. Lille University Hospital came out on top with 30.99 days, all causes combined.
By April 2022, 60 hospitals had triggered a white plan. Usually reserved for disaster scenarios, it was indeed on the basis of extreme staff fatigue that these plans were triggered. It allows non-urgent operations to be deprogrammed. A state of affairs which speaks volumes about the current situation in which nursing staff find themselves. This is the first time that a white plan has been triggered due to staff absenteeism.
I. Causes of hospital staff absenteeism

Work-related factors
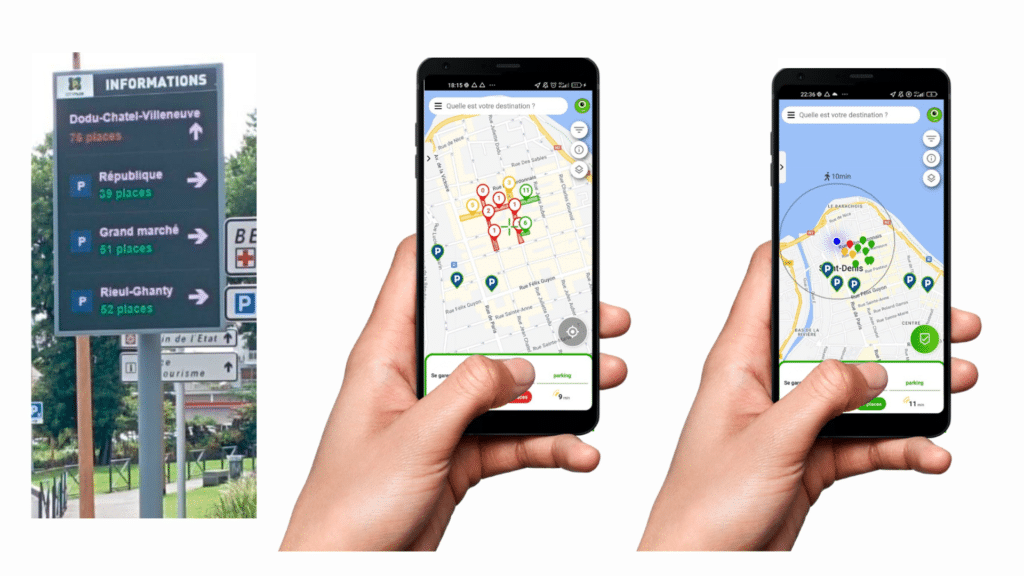
Excessive workloads are a major contributor to absenteeism. This article bears witness to working conditions that are harsher than elsewhere. Stress and burnout are major causes. In addition, the search for parking spaces on hospital sites that are far too often saturated only exacerbates the stress already present. Nurses at Strasbourg’s CHU(civil hospital) spoke of their situation: every morning, up to 45 minutes are wasted looking for a parking space on site, a situation that can no longer be allowed to continue. Physical and psychological working conditions also play a crucial role. Irregular working hours and stressful working conditions increase the risk of absenteeism.
“This rhythm breaks people down. From now on, they can break down over something stupid. There’s a lot of burn-out.”
Pascale Jacq, Sud Santé.
Personal factors
Health problems are a frequent cause of absenteeism. Family or personal conflicts can also prevent caregivers from getting to work. Chronic health problems or major family responsibilities are often contributing factors.
Organizational factors
Lack of managerial support is an important factor. Job dissatisfaction and a negative organizational culture increase absenteeism. Poor communication within the organization can also exacerbate the problem. In a survey of 4 hospitals conducted by two management science researchers, presenteeism was cited as the “dark side” of absenteeism. By overtaxing internal resources to make up for short- and long-term absences, this leads nurses to be more present in the field than they should be.
The Covid 19 crisis
Cases of contamination have multiplied among hospital staff, who were at the forefront of the Covid 19 crisis. Hospital managers are forced to review the organization of their teams on a daily basis. A real headache for departments already stretched to the limit in the middle of an epidemic wave.
II. Effects of staff absenteeism on hospital operations

What are the consequences for quality of care? ?
Absenteeism reduces the quality of patient care. The workload increases for the staff present, leading to additional stress. The absence of a healthcare professional disorganizes a department and directly threatens patient care and service quality. Disrupting or interrupting the care chain can have consequences for people’s health. This can lead to medical errors and a reduction in the overall quality of care.
Organizational consequences
Teams and departments are disrupted by absenteeism. Stress and demotivation among staff increase, affecting efficiency. High staff turnover can also lead to a loss of specific skills and knowledge. There’s also talk of “resourcefulness”, where lack of resources and time means that staff organize themselves as best they can to adapt to situations. As a result, the health executive is highly responsive and inventive when it comes to managing absenteeism on an urgent basis.
What are the financial consequences of absenteeism?
Absenteeism has a financial cost for healthcare establishments, whether direct (wages for replacements) or indirect, such as adaptation time. By way of example,Anact estimated “all costs linked to disruptions and additional costs linked to regulations” at €499,773 for a company with 180 employees in 2019. Direct costs include temporary replacements and overtime. Indirect costs include lost productivity and reduced patient satisfaction. Absenteeism has a significant impact on the hospital budget, increasing operating expenses. This is because absent staff are replaced by temporary staff or short-term contracts, adding to the costs, which are higher than those of the original staff under normal circumstances.
III. Solutions to reduce absenteeism in hospitals
Improving working conditions
Reducing workload is essential to reducing absenteeism. Setting up psychological support programs can help. Better team management is also crucial. For example, optimizing task allocation and offering more flexible working hours can be beneficial. This is what Skello offers, a solution that enables better planning, optimization and management of teams through easy-to-use software that centralizes data and is very user-friendly.
Using an application
The danger is that, when an agent is absent and needs to be replaced, the reflex is to work through a network. By always contacting the same caregivers, the most reactive, there’s a risk of inequity, and the danger is that the effort will fall on the same pool of people without respecting the work-life balance.
At Saint-Etienne University Hospital, we’ve set up an app that can be activated at will. This avoids the use of calls, sms and e-mails, which are more intrusive. Based on an algorithm, it analyzes the requested mission and cross-references it with the database containing the profiles’ characteristics. Depending on location, skills and availability, it makes an offer to several volunteers. The offer is withdrawn as soon as a positive response is received.
Strengthening managerial support
Training managers to manage stress and employee well-being is essential. Creating a culture of support and recognition can reduce absenteeism. Well-trained managers can better understand and respond to their teams’ needs, improving morale and retention. This is what the French Ministry of Health proposes in its guide“Mieux manager pour mieux soigner, améliorer le management et la gouvernance hospitalière“.
Financial measures
Investing in prevention initiatives pays off in the long term. According to a study by the Institut Sapiens, the average direct and indirect cost of absenteeism at work, whatever the sector of activity, amounts to 4,059 euros per employee each year, or around 107.9 billion euros for the working population in France. A real loss of earnings for a hospital. By reducing absenteeism in hospitals by just 0.5%, we save 1.3 million euros per year.
For example, the smart parking system deployed by Cocoparks can reduce parking-related stress. Cost-benefit analysis of programs to reduce absenteeism shows substantial gains.
Conclusion
Absenteeism among hospital staff has multiple causes and significant effects. Solutions include improving working conditions, strengthening managerial support and targeted financial measures. Investing in reducing absenteeism is crucial for the well-being of caregivers and the quality of care. A proactive and comprehensive approach is needed to tackle this problem effectively and sustainably.



